1. High numbers of autistic people experience co-occurring OCD.

We know this is a key area of training given that autistic people are twice as likely to also experience OCD. People with OCD are also four times more likely to be autistic. There is therefore a strong association between the two conditions (Meier et al., 2015).
Things started to feel quite overwhelming at school, with the GCSE’s and pressures to socialise with friends. There was a lot going on, I wanted to fit in but was struggling. There was a lot of uncertainty, things felt out of control. When I first found OCD, it felt so good – something I could control and rely on. But then it took over every hour of every day to the point where I couldn’t do or think about anything else. It got to the point where I couldn’t get into school. This was a very distressing and lonely place to be. The trigger was definitely all the changes at school, the uncertainty and feeling overwhelmed.
Young autistic man aged 18
2. OCD is a serious distressing condition.
OCD is defined as obsessions and/or compulsions which occupy more than 1 h/day (APA, 2013). Obsessions are understood as intrusive, persistent, and recurrent thoughts, images or impulses causing marked distress. Compulsions are behaviours or mental acts used to respond to or prevent imagined threat or harm.
Whilst performing rituals or compulsions may bring perceived relief from the distress caused by the obsessions – the relief is only temporary and re-occurs each time the obsessive thought, fear or worry is triggered.
Many autistic people with co-occurring OCD may be engaged in distressing and repetitive compulsions (rituals) that can overshadow their day and night and have a serious impact on their mental and physical well-being. High number of autistic people also report experiencing just right OCD where movements and thoughts need to be completed in a certain way and repeated until they feel, “just right.”
3. OCD affects every part of a person’s life with significant health risks.

OCD compulsions can prevent an autistic person from getting to school, university or work, engage in their interests and have friendships or relationships. There can be significant health risks associated with OCD where a person cannot get out of bed, move, take care of their personal hygiene, eat food, or attend medical appointments. This can lead to serious physical health conditions, life threatening risks including severe restricted eating patterns (e.g. due to OCD contamination beliefs related to food). Longer term OCD can be a barrier to living independently if left untreated.
4. It can be difficult to identify the overlaps and differences between autistic traits and OCD traits.
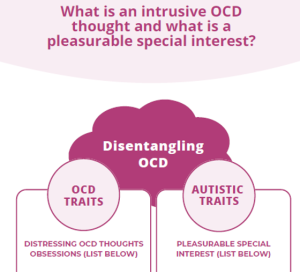
There can be similarities in the behavioural topography of OCD and autistic traits leading to challenges in identifying and separating out what experiences may be associated with OCD and those which are part of the autistic person’s neurodevelopmental profile.
Where a trait may be associated with an individual’s neuro-developmental profile such as stimming for sensory and emotional regulation, it’s important to recognise its meaning and value to the individual.
5. Autistic people may not have access to treatment for co-occurring mental health conditions.
Being autistic should not be a barrier to OCD treatment. Increasing understanding about the overlaps and differences, alongside access to neuro-affirmative tools and approaches will help to increase practitioner confidence in spotting the signs of OCD alongside providing timely access to referral and treatment.
6. OCD significantly affects family life and well-being.

It is also important to understand the wider impacts of OCD on families and siblings. Family members relationships, lives and mental health and well-being may be significantly impacted by OCD symptoms (Browning’s et al., 2023). Family members and siblings of OCD affected children and young people report feeling stressed and anxious.
OCD often exerts immense control over family lives through seeking reassurance and requiring family members to participate in compulsions. Whilst challenge may be seen as positive the impact of pulling back against OCD compulsions or not participating in routines can lead to massive emotional unrest within a household.
Recognising these challenges, is an important part of supporting families as autistic people with co-occurring OCD begin to navigate treatment options.
For more information about Autism and OCD training please click here

